Partners Well-Being
Congratulations on becoming a parent. Here is a booklet that you may find useful. It has lots of advice and activities (interventions) that could be of benefit to you during your transition into parenthood. If you would like to work through the booklet and would like to discuss or be supported through this, please contact a member of the Specialist Mother and Baby Mental Health Service (SMABS) team.
We wish you all the best in your transition into parenthood.
-
Your relationship with your partner
Becoming a parent changes relationships and, although this is normal, it can be hard.
Try to talk to your partner about how you are both feeling, to gain a mutual understanding. Talking to each other gives you a chance to find out about anything that you or your partner is finding difficult or worrying.
As new parents, you will both be tired, and you both will need to get rest. It is intense to look after a baby and whoever is the main carer for the baby will need a break and a rest. A lack of sleep can have an impact on your mood and affect day-to-day life. Try to manage this by asking for support, if available.
Bonding with your baby
Studies show that the quality and quantity of baby-mother and baby- father contact has a direct impact on how secure children feel growing up. Being as hands-on as possible helps your bonding with your baby. Daily tasks like nappy changing, winding, bathing and feeding, are all opportunities to be with your baby, chat, play games and enjoy your relationship. Talking and playing with your baby is a great way to build up a relationship, as this is what the baby enjoys.
You can find out lots more information that will help you understand your baby at Ready to Relate – Bradford District Care NHS Foundation Trust https://readytorelate.bdct.nhs.uk/ – or use this QR code and you can ask your health visitor, family hub or mental health practitioner to tell you more about Ready to Relate too.
-
Roles and routines
It can take time to adjust to becoming a parent, especially as some parents balance other roles such as being a worker. Babies take up a lot of time. For a while, you may find that your life begins to revolve around the baby. It can be useful to inform yourself as to what babies like and dislike at different stages. In the early months some tasks, like shopping, cooking, cleaning, even eating (!) may feel much trickier.
It takes time to adjust to a new routine after having a baby. You and your partner may have less time to do the things you enjoy. Working together so you both have some time to do activities on your own and activities that you enjoy together is great, but it may take some time to work out how to make this possible.
Structuring your routine
Things that we enjoy are good for our mental health. It could be useful to structure your daily routine to include a good balance of work, leisure and self-care as well as caring for and spending time with your baby. This can avoid you becoming overwhelmed and stressed. It is also useful to remember that as your child gets older it will become easier to get this mix in your life. Lack of sleep can have an impact on your mental wellbeing. Finding time to rest is important but can be a challenge with a new baby, try to work out a routine with your partner so you can both get the rest you need.
Breaking tasks down into smaller chunks can make them feel more manageable and help you feel less overwhelmed. Pacing yourself throughout day and taking advantage of the times when you have the energy to complete small jobs can help you when you aren’t feeling your best.
Wider family
Remember to communicate with your wider family so they can offer support. It can be easy to isolate yourself and reject help when you’re struggling but this may give you the time to reflect on your needs.
Our top tips for secure parent infant relationships
- Babies are born ready to relate and they are communicating, look out for their non-verbal cues.
- Cuddling and stroking your baby helps their brain
- When your baby turns away during play it can be a sign they need to slow down.
- Babies have their own personality, enjoy getting to know your Wonder to yourself about what might be going on in your baby’s mind.
-
When you are feeling low, it is normal to think “why me? Am I the only one who feels like this? Why is life so difficult?”
You may have returned to work, meaning you have less time to spend with your baby and partner, which you expected to be a very exciting time in your life. This is a very common but difficult adjustment for most parents.
Feelings of low mood and anxiety are common in fathers during the perinatal period (which is classed as pregnancy and up to 1 year following birth). Studies completed by MIND into postnatal depression in fathers suggest that around one in five men experience depression after having a baby. In the UK, men are three times as likely to die by suicide.
If your partner is struggling with their mental health, it can be even more difficult to share how you’re feeling with them. It is important to reach out for support for yourself, as well as your partner if it is needed.
The NHS mood tracker is useful to measure your stress and mood and can help you understand how you are feeling. It can also provide advice on ways to get support.
If your mood is low, or you feel anxious, please make an appointment with your GP. Medication and talking therapies can be helpful. Exercise can also help. Taking care of yourself with sleep and diet is important too. There are services there to help you. Speaking with your GP will help you identify what is best for you.
-
When you are feeling stressed, anxious or low in mood, you act in different ways in order to cope with this. Everyone copes in different ways, some of which can cause more harm to your mental health.
Take time to consider, what do you like to do to unwind after a difficult or stressful day?
Positive coping mechanisms:
- Exercise
- Mindfulness
- Grounding techniques
- Speak to a friend/family
- Play with your baby
Negative coping mechanisms
- Alcohol use
- Drug use
- Gambling
- Too much time on social media
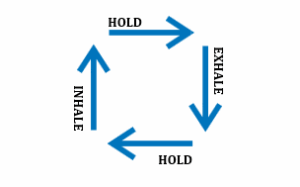
Grounding techniques can be used to ease anxieties and allow yourself to feel calmer. Examples include rainbow counting and box breathing:
- Rainbow counting focuses on looking for colours around the room, to help distract your mind.
- Box breathing focuses on using deep, long breaths to relieve
Alcoholics Anonymous Phone: 0800 917 7650 Website: www.alcoholics-anonymous.org.uk
National Gambling Helpline – Phone: 0808 8020 133 Website: www.begambleaware.org
Narcotics Anonymous – Phone: 0300 999 1212 Website: www.ukna.org
Talk to Frank
-
Our brains are very alert to try to keep us safe. Parts of our brain are focused on detecting threat and then taking action to keep us safe. A part of our brain which is part of our threat system is called the amygdala. It alerts us to danger and sets off the alarm in our body if it detects any danger. This alarm triggers our flight, fright, freeze system, which helps us to take the action we need for our safety.
-
Our amygdala can sound the alarm in our brain:
- to save us from very serious threats,
- it can also sound the alarm when we are stressed,
- when we have worrying thoughts or relationship stresses, when we are worried about not belonging in a group,
- by things our brain has learnt to associate with a trauma, like a particular smell or sound,
- and sometimes we just don’t know what set it off, after all everybody’s brain makes plenty of mistakes!
When our brains have detected threat, our brain is so focused on our safety that sometimes other parts of the brain don’t work so well. For example, a part of our brain called the hippocampus is involved in the storage of memories, but when we are experiencing threat it sometimes does not work so well. Later when we remember an experience that was a threat – a memory – sometimes it feels like it is happening again, rather than it being clear that that was in the past and we are safe now.
If you are feeling stressed because of a trauma there are therapeutic interventions that can help. There are also strategies that you can use to help soothe your brain and relax your body.
For some people, their flight, fight, freeze safety system will be set off because they are feeling stressed, because they are experiencing lots of worries, or lots of change. There are interventions which can help manage anxiety. There are also strategies which you can use to help to soothe your brain.
-
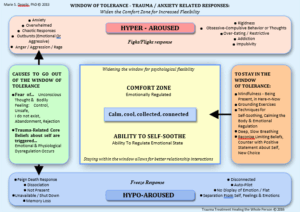
We each have a window of tolerance. We are in our window of tolerance when we feel safe enough. When we feel safe, we feel calm. We can manage problems as they crop up and they pass.
But people can only cope with a certain amount of stress at any one time. We only have a certain amount of resilience. People can cope with different amounts of stress, some of this is genetics, some of this is about the amount of support they have, some of this is about the types of stress, some of this is about the strategies they can use and some of this is about how safe their brain generally feels. For example, someone who has experienced lots of trauma may have a brain that already feels less safe than someone who has not experienced lots of trauma.
When our brain detects too much threat we come out of our window of tolerance and our flight, fight system may be activated – we are hyper- aroused, or our freeze system may be activated – we are hypo-aroused.
When we are hyper-aroused we may feel anxious, overwhelmed, angry, we may be chaotic, impulsive, have outbursts, we may have habits that are not healthy for us but that we use to help us feel less scared, or more in control.
When we are hypo-aroused we may feel numb, disconnected, unemotional, disassociated, flat, not present, and our memory may not work so well, we may feel like we are on auto pilot.
We can try and calm our brain in different ways to help us get back into our window of tolerance.
-
Helping your brain know that right now you are safe
Step one:
Controlled shaking to help soothe anxiety
When you feel very anxious, stressed or fearful, you may notice that you start to shake or that you feel agitated, like your body is telling you to move.
What to do: controlled shaking ideas
If you are sitting, tap your feet and bounce your knees more than you normally would. If you are alone, stand and shake your body out. Shake your hands and arms. Sit down and shake your legs. Give your torso a wiggle. Move your head side- to-side.
Even better, put on some music that gets you dancing. Shake each leg and bounce on your toes like you see sprinters do before a race.
Shake it out, shake it off.
Why: shaking out anxiety
Shaking from anxiety is nature’s way of de-stressing.
In the wild, when an animal has just avoided an attack, it will shake intensely for several minutes and then return to eating grass as if nothing has happened – it’s part of the fight or flight response.
This shaking allows it to release the build-up of stress hormones that occurred during the “anxiety attack”.
We often suppress shaking and tense up instead – it is as if we keep that energy locked in when it wants to get out by movement.
Shaking is a part of the fight-or-flight response
When you’re extremely anxious, your body activates a fight-or-flight response to danger, even when no real danger is present.
This response triggers a rush of adrenaline, which feeds your body with energy, arouses your nervous system and prepares to be able to fight or flight.
Shaking is a sign that your body is releasing energy. It happens when your fight-or-flight response winds down.
By choosing to shake your body you can discharge this energy faster. Exaggerate shaking.
Step two:
Safe brain breathing
What to do: a gentle, longer breath out
Pause.
Just gently breathe out. Take a moment. Don’t breathe out fast and hard. Imagine you have a line of birthday candles in front of you and all you want is for your out-breath to gently bend the flames of these candles. You are not trying to blow the candles out.
Pause again.
Repeat a few times.
By breathing out in a gentle way you are helping your breathing to begin to balance out. If you were running away from a sabre-toothed tiger you would not be breathing gently out! This gentle breath helps trick your brain into thinking you are safe.
Why: flight and fight breathing to safe breathing
When we are in danger our breathing changes. We breathe quickly so we get lots of oxygen into the body to help us be ready to run from the danger. You may find your body is telling you that you need to get more oxygen.
Sometimes you may become very attentive to your breathing – usually we breathe outside of our awareness and by paying lots of attention to it we alter the rhythm and start to over-breathe.
Even though you are over-breathing your body is so focused on danger that it tells you that you need to breathe more oxygen in and so you keep over-breathing.
You may notice these symptoms:
- Rapid heartbeat.
- Difficulty concentrating.
- Shortness of breath.
- Weak or tingling limbs.
- Chest pains.
- Light-headedness/feelings of faint.
These may worry you and so you feel more in danger and over-breathe more.
A gentle slow breath out helps your brain feel safe.
Step three:
Build the habit of telling your brain that you are safe.
Get into the habit of doing step one and two
Your brain may be in the habit of telling yourself you are in danger. You are building a new habit of telling your brain you are safe. You can tell yourself out loud that you are safe when you start and finish step one and two.
Building habits takes repetition so try a reminder on your phone to do the steps or try to do them before you have a cup of tea, or after you have done a regular task like changing a nappy.
By building a habit of telling your brain you are safe the anxiety doesn’t build up and catch you out, rather you soothe your brain.
-
- Sit in a comfortable chair (or lie on the floor, or on a bed). Ensure you will not be disturbed by other noises. If you become aware of sounds – just try to ignore them and let them leave your mind just as soon as they enter.
- Make sure the whole of your body is comfortably supported – including your arms, head and feet. (Rest your arms on the arms of the chair, with your feet flat on the floor – if sitting!).
- Close your eyes. Feel the chair supporting your whole body – your legs, your arms, your head. If you can feel any tension, begin to let it go. Take two slow and deep breaths, and let the tension begin to flow out.
- Become aware of your head – notice how your forehead feels. Let any tension go and feel your forehead become smooth and wide. Let any tension go from around your eyes, your mouth, your cheeks and your jaw. Let your teeth part slightly and feel the tension go.
- Now focus on your neck – let the chair take the weight of your head and feel your neck relax. Now your head is feeling heavy and floppy. Let your shoulders lower gently down. Your shoulders are wider, your neck is longer.
- Notice how your body feels as you begin to relax.
- Be aware of your arms and your hands. Let them sink down into the chair. Now they are feeling heavy and limp.
- Think about your back – from your neck to your hips. Let the tension go and feel yourself sinking down into the chair. Let your hips, your legs and your feet relax and roll outwards. Notice the feeling of relaxation taking over.
- Think about your breathing – your abdomen gently rising and falling as you breathe. Let your next breath be a little deeper, a little slower.
- Now, you are feeling completely relaxed and heavy. Lie still and concentrate on slow, rhythmic breathing.
- Then you want to count back from five to one and open your eyes. Wiggle your fingers and toes, breathe deeply and stretch. Pause before gently rising.
-

-
Tip the temperature of your face with cold water (to calm down fast)
- Holding your breath, put your face in a bowl of cold water, or hold a cold pack (or zip-lock bag of cold water) on your eyes and cheeks.
- Hold for 30 seconds. Keep water over 10°C (Only suitable for adults).
Intense exercise (to calm down your body when it is revved up by emotion)
- Engage in intense exercise, for a short while: running, walking fast, jumping, playing basketball, lifting weights, etc.
Paced breathing (pace your breathing by slowing it down)
- Breathe deeply into your belly.
- Slow your pace of inhaling and exhaling way down (on average, five to six breaths per minute).
- Breathe out more slowly than you breathe in (for example, 5 seconds in and 7 seconds out).
Paired muscle relaxation (to calm down)
- While breathing into your belly deeply tense your body muscles (not so much as to cause a cramp).
- Notice the tension in your body.
- While breathing out, say “relax” in your mind.
- Let go of the tension. Notice the difference in your body.
-
When we are feeling overwhelmed or anxious it might be a good time to STOPP. Why don’t you give it a go?
Stop
Take a breath

Observe – describe the feelings, images, thoughts, body sensations, triggers.
Pull back / Put in some Perspective. What’s the bigger picture? Take the helicopter view. Is this fact or opinion? How would someone else see this? Is there another way of looking at this?
Practice what works. What is the best thing to do right now – for me, for others, for the situation.
-
When we are stressed we are less able to empathise with others and less good at seeing others’ perspective. It is important to remember that babies and children cannot understand what you are experiencing and cannot know what to do for you.
Babies and children need sensitive, good enough parents. Babies and children often want to be close to their parent. They are very good at picking up other people’s stress and although they do not understand it, it can worry them. When a baby or child is worried, they feel stressed and their alarm system may be set off too. Then they may be in their flight, fight, freeze system too – both of you are in your alarm systems! This often results in more frustration.
Babies and younger children don’t have the brain development to manage their own emotions and they need you to soothe their brain. For example, talk calmly or sing, give your baby skin to skin, hold them close, have a warm bath, go for a walk outside. As children get a little older, some of the exercises in this leaflet may be helpful for them too.
If you feel that you are unable to cope or you are becoming angry with your baby or child, take a moment:
- Move away from your child if necessary and practice STOPP.
- Remember your baby does not mean to upset or anger you.
- Try to understand their perspective and experience.
- Ask a friend or relative for some support.
- Soothe your brain and soothe their brain. Use some exercises from this leaflet.
-
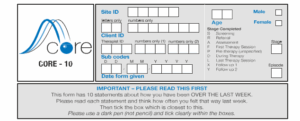
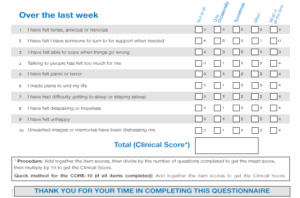
If you are concerned about your mental wellbeing, you could complete the Core 10 screening measure below. If you score 10 or above or have any thoughts of suicide or harm to yourself or another, then please contact your GP for further support and advice. If you feel that you are experiencing a mental health crisis, please contact First Response 0800 952 1181.
-
If you are struggling, then speak to your GP or another healthcare professional. There are several organisations and groups available, that can offer you peer support and guidance.
Bradford Mind
- Email: admin@mindinbradford.org.uk
- Website:www.mindinbradford.org.uk
- Telephone:01274 594 594
Bradford District and Craven Talking Therepies
- Website: www.bdctalkingtherapies.nhs.uk
- Telephone:01274 221234
- Write to us: Bradford District and Craven Talking Therapies, Bradford District Care NHS Foundation Trust, Level 5, New Mill, Victoria Road, Saltaire, BD18 3LN
The Birth Trauma Association
- Website: The Birth Trauma Association
Bradford Council
- Website: https://www.bradford.gov.uk/EarlyHelp
Best Beginnings/ Out of the Blue
- Website: www.bestbeginnings.org.uk/out-of-the-blue
- Facebook: www.facebook.com/bestbeginningscharity
Andys Man Club
- Website: www.andysmanclub.co.uk
- Facebook: AndysManClub
- Instagram: @AndysManClubUK
- Twitter: @AndysManClubUK
Every Monday at 7PM (except bank holidays)
Bradford: Millside Centre BD1 2HS
Leeds: Leeds College of Building North Street Leeds LS2 7QT
CALM:
Campaign Against Living Miserably, for men aged 15-35.
- Website: www.thecalmzone.net/
- Telephone: 0800585858
NCT
Carers Resource
Bradford : 15 Park View Court, St Paul’s Road, Shipley BD18 3DZ Tel: 01274 449660
Harrogate: 11 North Park Road, Harrogate HG1 5PD Tel: 01423 500555
Skipton: Ronaldsway House, 36 Brook Street, Skipton BD23 1PP Tel: 01756 700888
DadPad
Website: www.thedadpad.co.uk
The Equity Partnership – Equity Centre 1 Longlands Street, Bradford, West Yorkshire.
- Telephone: 01274 727759 or 07404840598
- Email: lgbtkeighley@gmail.com admin@equitypartnership.org.uk
- Website: www.equitypartnership.org.uk
Family lives
- Website: Parenting and Family Support | Family Lives
- Telephone:08088002222
Pride and Joy playgroup
Facebook: www.facebook.com/Prideandjoyplaygroup
Proud 2B parents
- Telephone: 07843913001
- Website: www.proud2bparents.co.uk
It’s worth talking about Mondays 6.30-8.30pm Hop on Worth
24 Cavendish Street, Keighley Industry Barista, 5 Mill Hey, Haworth
Yorkey dads
Dads group based in York, also offers online support.
- Website:yorkeydads.co.uk
- Twitter: @YorkeyDads
- A timetable of groups in Bradford, Airedale and Craven: https://www.betterliveshealthyfuturesbw.nhs.uk/information- zone/
Anxiety UK
Provides support if you have been diagnosed with an anxiety condition.
- Phone:03444 775 774
- Website: www.anxietyuk.org.uk
Men’s Health Forum
24/7 stress support for men by text, chat and email.
Website: www.menshealthforum.org.uk
Samaritans
Confidential support for people experiencing feelings of distress or despair.
- Phone:116 123
- Website: www.samaritans.org
SANE
Emotional support, information and guidance for people affected by mental illness, their families and carers.
- Textcare: support via text message, sent when the person needs it most:www.sane.org.uk/textcare
- Peer support forum: www.sane.org.uk/supportforum
- Website: www.sane.org.uk/support
- SANEline: 0300 304 7000
If you have been affected by baby bereavement the charities below are able to offer both emotionally and practically support during these difficult times.
Forget me not children hospice
- Phone: 01484411042
- Email: care@forgetmenotchild.co.uk
Sands
- Phone:08081643332
- Email: helpline@sands.org.uk
-
The team’s contact number is 01274 221180, please ask the call handler to be put you through to Specialist Mother and Baby Mental Health Service. If you have anything important that you want to share, please use this number.
If you experience a mental health crisis, please call First Response on 0800 952 1181.
Ready to Relate – Bradford District Care NHS Foundation Trust provides information to help you understand your baby and develop your bond with them. https://readytorelate.bdct.nhs.uk/