Pain in your heel – fat pad syndrome
Pain in your heel – fat pad syndrome
What is fat pad syndrome?
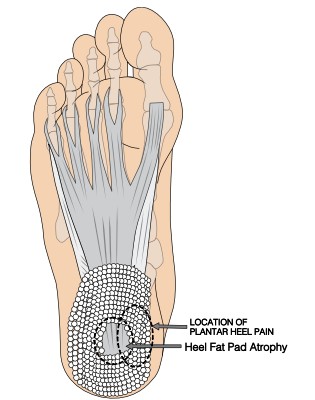
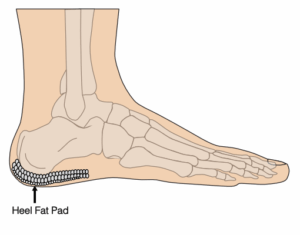 Fat pad syndrome (also known as heel fat pad atrophy) is a thinning of the plantar fat pad, the soft tissue layer in between the skin and heelbone that supports and cushions your heel.
Fat pad syndrome (also known as heel fat pad atrophy) is a thinning of the plantar fat pad, the soft tissue layer in between the skin and heelbone that supports and cushions your heel.
The fat pad has a honeycombed structure of fibro elastic chambers containing fat globules which help with shock absorption and spreading pressure across the surface of your heel during activity. When the fat pad thins, reduced shock absorption makes the heel bone more vulnerable to repetitive microtrauma, leading to chronic inflammation, bruising, swelling and pain within the heel bone.
Increased load can also lead to irritation and inflammation of the bursa (small fluid filled sack) which sits under the fat pad between the heel bone and the soft tissue. This bursa also helps with shock absorption and reducing friction.
Signs and symptoms of fat pad syndrome
 A gradual onset of a dull achy pain under the centre of the heel.
A gradual onset of a dull achy pain under the centre of the heel.- Pain increases with activity during periods of standing or walking.
- Localised swelling that can cause discomfort when wearing footwear.
- The heel can feel tender or warm and is more painful when you press directly on it.
Symptoms can appear very similar to those of plantar heel pain, but with your initial first steps in the morning and after periods of rest, the discomfort is not as painful, the pain tends to build with increased weight bearing activity.
What causes fat pad syndrome?
In most cases, fat pad syndrome develops as a result of repeated overuse.
Other contributing factors include:
- being overweight
- age – there is a natural thinning of the fat pad for people aged over thirty
- wearing inappropriate unsupportive footwear (see our footwear advice page)
- spending long periods standing or walking, especially with a sudden increase in these activities
- diabetes
- inflammatory conditions, such as rheumatoid or psoriatic arthritis
- weakness in the muscles within your feet or leg
- tightness of the muscles in the backs of your legs
- not allowing adequate recovery time between activities
- prolonged use of oral corticosteroids
What can I do to relieve the pain of fat pad syndrome?
There are a number of things you can do to reduce the pressure on your bunion – this will not correct the deformity or change the size or shape of the bunion, but it will help to relieve pain. Making changes to your lifestyle so you reduce aggravating activities is key.
Things to try:
- raising your foot on a stool and resting it when you can
- putting an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every two to three hours
- shoes with cushioned heels and good arch support
- insoles in your footwear
- regular stretching and foot exercises
- exercises which put no pressure on your feet, such as swimming
- losing weight if you’re overweight or obese.
Things to avoid:
- walking or standing for long periods
- wearing high heels or tight, pointy shoes
- wearing flip-flops or backless slippers
- walking barefoot on hard surfaces.
Ankle, foot and toe rehabilitation exercises
The video exercises shown below will help to improve your pain over a period of time. Watch the video first, then try the exercise. There are nine videos to try – go through to the next one below by clicking the arrow on the right of the video. All videos provided and shared with kind permission of, and thanks to, the Musculoskeletal Podiatry team at NHS Lanarkshire.
You need the use of a clear space of wall, a small towel, a small plastic bottle of water, a sports resistance band and a sports therapy ball. If you do not have a sports resistance band or sports therapy ball (also known as a soft spiked massage ball) these can be purchased relatively inexpensively online. If cost is an issue, focus on the exercises which do not use that equipment.
Important – pain levels: the NHS uses a pain scale where pain is measured from 0-10 (zero being no pain and 10 representing the worst pain you could imagine).

If you can identify the level of pain you are experiencing, you will find out if you are in the green, amber or red zone.
When you are completing your rehabilitation exercises it is often best to work within the green (and sometimes amber zones depending on what you deem is an acceptable level of pain) both during the exercises and within 48 hours of completing your exercises.
The best way to move down to the green zone is by pacing and spacing your activity. If you find yourself in the red zone you are likely pushing yourself too hard and the pain may flare up.
If you notice a large increase in your pain after doing the exercises, or you find that after six to twelve weeks there is no noticeable changes in your day to day symptoms, then please contact your GP or self-refer to our MSK podiatry team.