Pressure ulcers – guide for patients and carers
Pressure ulcers – guide for patients and carers
This quick and easy to follow guide is for patients and carers. It explains what a pressure ulcer is, what causes it and how to check for and prevent pressure ulcers.
What is a pressure ulcer?
Pressure ulcers (also known as pressure sores or bed sores) are areas of damage to the skin and the tissue underneath. There is a higher chance of getting a pressure ulcer if you have difficulty moving.
Pressure ulcers usually form on bony parts of the body, such as the heels, elbows, hips and tailbone. They usually develop gradually, but can sometimes appear over a few hours. A pressure ulcer can become a blister or open wound. If left untreated they can get worse and eventually reach deeper layers of skin or muscle and bone.
You may find this video helpful:
How are pressure ulcers caused and who is at risk?
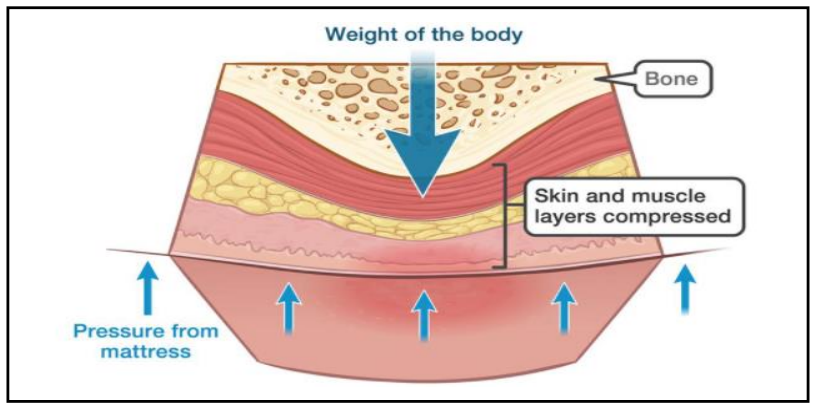 Pressure ulcers are caused by something putting pressure on or rubbing the skin. Anyone can develop a pressure ulcer, but its more likely if you have problems moving, as this can mean the weight of your body is always putting pressure on the same areas of skin, which can damage it. This is a higher chance of getting a pressure ulcer if you:
Pressure ulcers are caused by something putting pressure on or rubbing the skin. Anyone can develop a pressure ulcer, but its more likely if you have problems moving, as this can mean the weight of your body is always putting pressure on the same areas of skin, which can damage it. This is a higher chance of getting a pressure ulcer if you:
- are over 70 years old
- have problems moving or are confined to bed
- are incontinent
- have had a pressure ulcer before
- have been seriously ill in intensive care or have recently had surgery
- have poor diet or fluid intake, are underweight, or obese
- have swollen, sweaty or broken skin
- have poor circulation or fragile skin
- have problems feeling sensation or pain.
What are the symptoms of a pressure ulcer?
Early symptoms of a pressure ulcer include:
- part of the skin becoming discoloured – people with pale skin tend to get red patches, while people with dark skin tend to get purple or blue patches
- discoloured patches not turning white when pressed
- a patch of skin that feels warm, spongy, or hard
- pain or itchiness in the affected area.
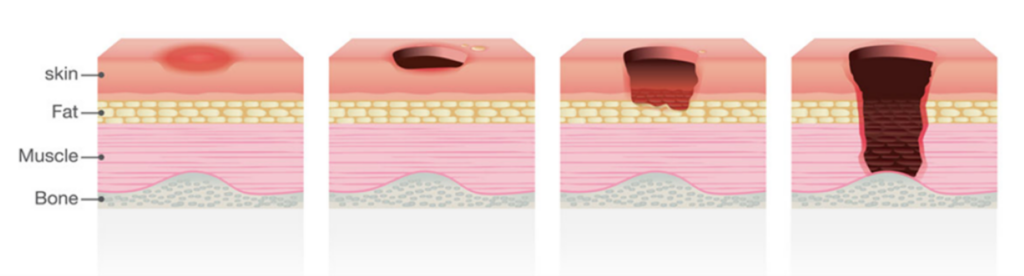
Later symptoms include:
- an open ulcer or blister
- a deep ulcer that reaches the deeper layers of the skin
- a very deep ulcer that may reach muscle, bone or tendon.
How to check for a pressure ulcer
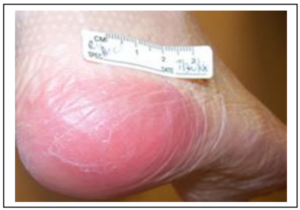 If you’re worried about a possible pressure ulcer, we advise moisturising dry skin to reduce the risk of skin damage and checking skin twice a day – especially bony areas. Look out for:
If you’re worried about a possible pressure ulcer, we advise moisturising dry skin to reduce the risk of skin damage and checking skin twice a day – especially bony areas. Look out for:
- any changes in skin colour – red patches on light skin, or bluish/purple patches on dark skin
- a bluish/purple bruise like discolouration – this may indicate possible damage to deeper layers
- any swelling, hard lump, squishy area of the skin, discomfort, or pain
- the area feeling hot to the touch or cooler than surrounding skin, the skin may itch too
blisters, either clear fluid or blood filled - any kind of damage/changes to your skin could increase the risk of developing a pressure ulcer.
If you’re struggling to check yourself, a mirror is a great way to check areas that are hard to see such as your bottom or back.
If you have Diabetes, this can affect the condition of your skin and slow down the healing process. Remember to check your feet and ensure that footwear isn’t too tight.
What to do if you see signs of damage to the skin or have concerns
It is important to contact your nursing team if you have any concerns or see any signs of skin damage. Without care, a pressure ulcer can become very serious and may lead to damage of the muscle, tendon, or bone underneath the skin. Pressure damage can take a long time to heal, and a serious pressure ulcer could lead to life threatening infections.
Tips for preventing pressure ulcers
Keep moving – changing position regularly is one of the best ways to prevent pressure damage. If you are unable to do this yourself, ask a carer, relative or friend to help.
Sitting and lying positions – please ask your nursing team for advice around correct sitting and lying positions, how to keep a good posture and how best to support your heels.
If you’re incontinent – it’s particularly important to keep skin clean and dry – use non-perfumed skin products, pat skin dry and don’t rub.
Eating and drinking – nutrition is important to keep skin in a healthy condition, so try to eat a well-balanced diet and drink plenty of fluids.