Pain in your heel – plantar heel pain (plantar fasciitis)
Pain in your heel – plantar heel pain (plantar fasciitis)
What is plantar heel pain?
Plantar heel pain, also known as plantar fasciitis, is the most common condition affecting the foot. One in ten people develop it at some point in their life, most commonly between the ages of 40 and 60. Women are twice more likely to develop plantar heel pain than men and it is also common in athletes.
Plantar heel pain is mainly due to mechanical overuse of the plantar fascia (see below). When pain develops here, it can be very disabling. Every step can become more painful and can cause you to change the way that you walk.
What is the plantar fascia?
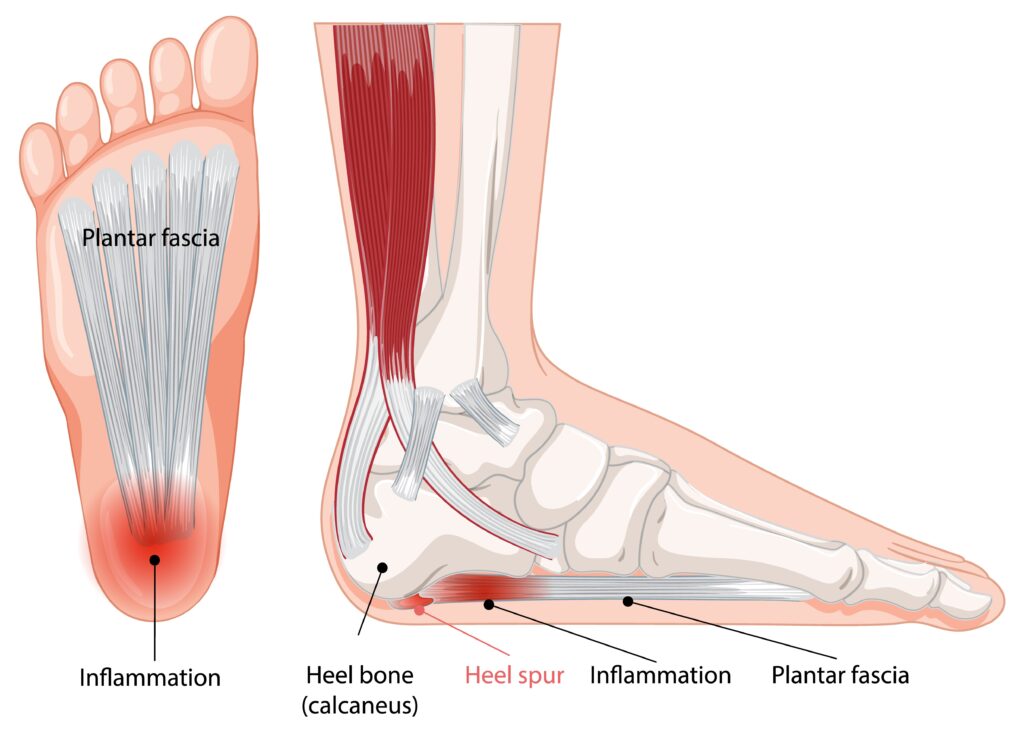
The plantar fascia is a thick band of tissue or “fascia” on the sole of the foot. It runs from your heel to the base of each toe and can be felt just underneath your skin. It helps to support the arch of your foot, and acts as a shock absorber, allowing the foot to take your body weight when standing, walking, running and carrying out weight-bearing exercises. The plantar fascia also stabilizes the foot to allow you to push off through your toes.
Excessive and repeated pressures, for example while running or walking with repeated foot impact on the ground, increases the stress on the insertion point of the plantar fascia, which can lead to microtears and microtraumas, triggering an inflammatory response and degeneration and thickening of the plantar fascia.
Microtraumas and inflammation boost the formation of bone cells responsible for heel spurs as the body tries to protect the area from the stress related to plantar fasciitis.
Signs and symptoms of plantar heel pain
You may experience any or all of these symptoms:
- a gradual onset of pain affecting the base of your heel
- pain in your heel during your first steps after getting out of bed in the morning
- pain in your heel when putting weight on it after a period of inactivity or rest
- pain that eases or lessens with moderate activity
- worsening pain later on during the day or after long periods of standing or walking.
What causes plantar heel pain?
In most cases, plantar heel pain develops as a result of changes to the way the foot functions, with small tears occurring within the plantar fascia. These injuries happen at a rate faster than the body can heal them and as a result the plantar fascia starts to become thickened and painful. The pain is most commonly felt under the inside of the heel but can be anywhere along the bands of the plantar fascia.
Other contributing factors include:
- being overweight
- weakness in the muscles within your feet or leg
- tightness in the muscles up the backs of your legs
- wearing unsupportive footwear such as shoes or sandals which have a low heel and don’t support the feet – you may find it useful to check out our footwear advice page
- spending long periods standing or walking, especially with a sudden increase in these activities
- jobs that involve standing or walking on hard surfaces for long periods of time
- sudden increase in physical activity levels – for example, if you recently started running.
What can I do to relieve plantar heel pain?
With appropriate advice and treatment the condition resolves for the vast majority of people, so you are encouraged to follow the advice and self-care exercises on this page before considering self-referral to the musculoskeletal podiatry team.
Unfortunately there is no quick or easy fix and your symptoms won’t improve overnight. However, if you have any of the contributory factors mentioned above, making necessary changes to your lifestyle and reducing aggravating activities can help your recovery. Only you can do this.
Things to try:
- raising your foot on a stool and resting it when you can
- putting an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every two to three hours
- shoes with cushioned heels and good arch support
- insoles in your footwear
- regular stretching and foot exercises
- exercises which put no pressure on your feet, such as swimming
- losing weight if you’re overweight or obese.
Things to avoid:
- walking or standing for long periods
- wearing high heels or tight, pointy shoes
- wearing flip-flops or backless slippers
- walking barefoot on hard surfaces.
Ankle, foot and toe rehabilitation exercises
The video exercises shown below will help to improve your pain over a period of time. Watch the video first, then try the exercise. There are nine videos to try – go through to the next one below by clicking the arrow on the right of the video. All videos provided and shared with kind permission of, and thanks to, the Musculoskeletal Podiatry team at NHS Lanarkshire.
You need the use of a clear space of wall, a small towel, a small plastic bottle of water, a sports resistance band and a sports therapy ball. If you do not have a sports resistance band or sports therapy ball (also known as a soft spiked massage ball) these can be purchased relatively inexpensively online. If cost is an issue, focus on the exercises which do not use that equipment.
Important – pain levels: the NHS uses a pain scale where pain is measured from 0-10 (zero being no pain and 10 representing the worst pain you could imagine).

If you can identify the level of pain you are experiencing, you will find out if you are in the green, amber or red zone.
When you are completing your rehabilitation exercises it is often best to work within the green (and sometimes amber zones depending on what you deem is an acceptable level of pain) both during the exercises and within 48 hours of completing your exercises.
The best way to move down to the green zone is by pacing and spacing your activity. If you find yourself in the red zone you are likely pushing yourself too hard and the pain may flare up.
If you notice a large increase in your pain after doing the exercises, or you find that after six to twelve weeks there is no noticeable changes in your day to day symptoms, then please contact your GP or self-refer to our MSK podiatry team.